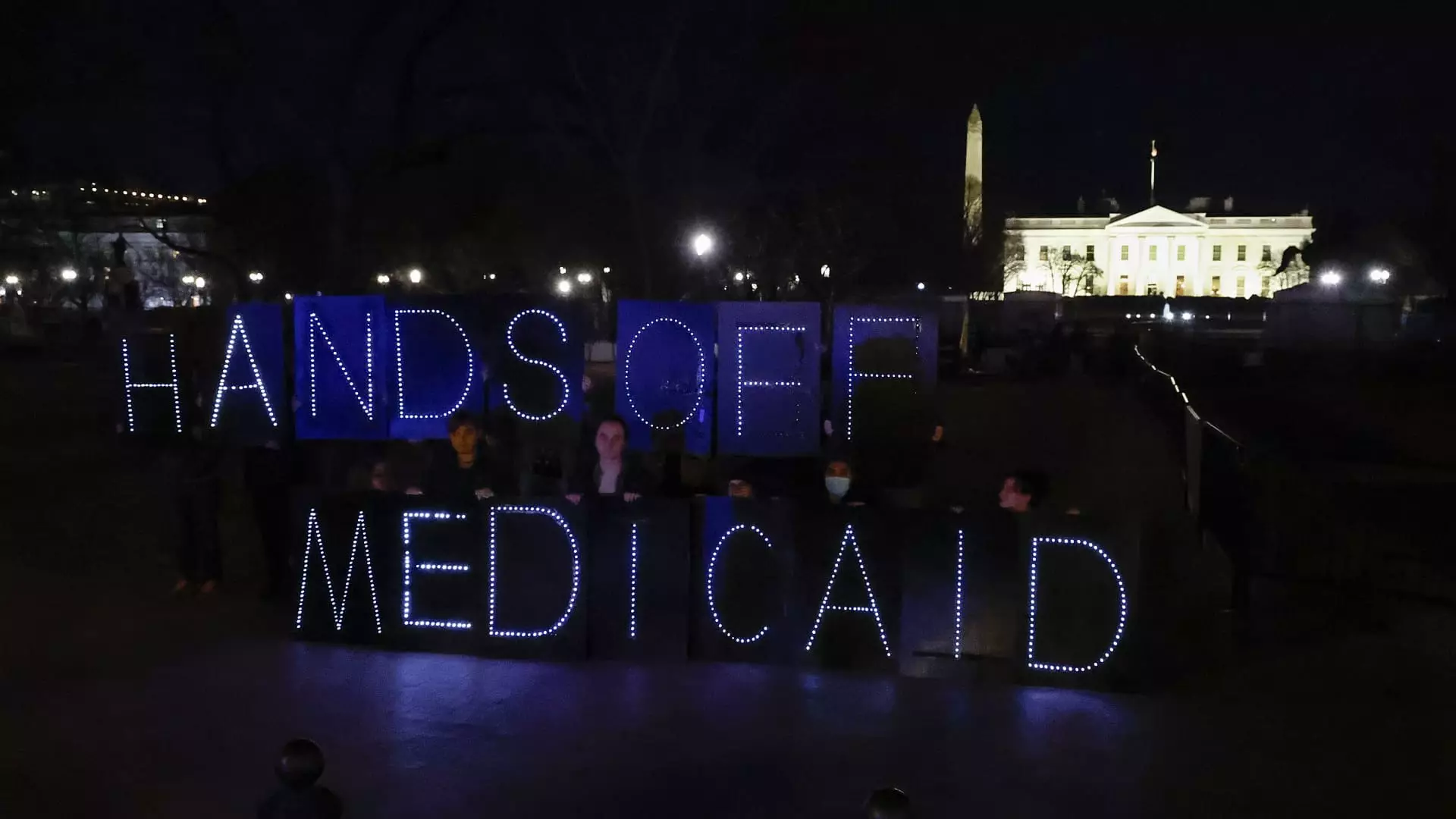
Recent revelations from the Congressional Budget Office (CBO) have painted a grim picture for the future of Medicaid in the United States. House Republicans, in a bid to adhere to their budget aspirations, are contemplating cuts that could slash as much as $880 billion from this essential program. Medicaid is not just a lifeline for the economically vulnerable; it covers critical health services for millions who rely on it for care that Medicare doesn’t provide, including nursing home services and long-term care. A large portion of the population—approximately 80 million people—depends on this program, and any changes could significantly disrupt their access to healthcare.
While there’s a vocal push from some factions within the Republican Party to introduce work requirements as a means to restrict Medicaid access, the premise is fundamentally flawed. According to the CBO’s findings, the proposed work mandates could lead to an estimated 36 million enrollees losing their healthcare coverage. This figure represents an alarming 44% of those currently enrolled in Medicaid, which raises critical questions about the morality and efficacy of using bureaucratic hurdles to determine one’s eligibility for essential health services.
The Work Requirement Debate
Proponents of the work requirement idea suggest it could decrease Medicaid spending and encourage personal responsibility. A recent poll indicated that around 60% of Americans are in favor of making work a condition for Medicaid eligibility. However, this public support may stem from a misunderstanding of both the program and the realities faced by enrollees. Many of them already juggle multiple jobs or struggle with obstacles that make accessing stable employment arduous.
The examples from Arkansas and New Hampshire serve as sobering cautionary tales. In Arkansas, where work requirements were implemented, nearly a quarter of those subjected to the rule lost their coverage within just seven months; their program was ultimately halted due to the fallout. New Hampshire saw similar failures, indicating a trend of disenrollment that raises alarm bells. This evidence suggests that rather than serving its intended purpose, work requirements would merely amplify the existing inequalities engrained within our social safety net.
The Failure to Address Structural Inequalities
Experts have pointed out the ideological differences that separate the U.S. from progressive European social democracies. As Farah Khan from Brookings Metro articulated, American attitudes toward social welfare are marred by a punitive lens that equates poverty with personal failure. This stance ignores the broader structural inequalities at play, such as systemic racism, education gaps, and economic disparities that leave many individuals in need of support.
Work requirement policies do not tackle these underlying problems; instead, they create new barriers to essential care. Laura Harker, a senior policy analyst, highlights how these administrative burdens disproportionately harm those who may be between jobs or possess disabilities. In fact, data shows that the vast majority of Medicaid recipients are already employed or exempt from work requirements—suggesting that imposing these mandates would essentially create unnecessary obstacles for those already striving to make ends meet.
The Economic Implications of Medicaid Cuts
The potential Medicaid cuts come at a critical time when healthcare officials warn of an impending crisis in access to care. Given that healthcare is an indispensable pillar for economic stability, diminishing access could have far-reaching implications not just for personal health outcomes but also for the overall economy. Cutting funding may lead to higher uncompensated care costs, which hospitals and healthcare providers inevitably pass on to taxpayers in the form of higher insurance premiums and fees.
Additionally, research indicates that imposing work requirements might not fulfill the intended outcome of incentivizing employment. Instead, it risks pushing people out of the safety net entirely, which could further strain state resources as uninsured individuals turn to emergency care. The healthcare landscape could shift dramatically, moving from accessibility to scarcity, creating a much larger issue for all of society.
The Path Forward: Rethinking Medicaid
As debates swirl and legislative proposals surface, we must call for a fresh perspective on Medicaid rather than adopting ineffective punitive measures. It is imperative that lawmakers acknowledge that social safety nets should not only be a generous provision but also a pathway for individuals to reclaim their place in society. Policies built upon compassion and understanding of the complexities of modern life will better serve those in need and ensure that the most vulnerable among us can access the healthcare they require.
Ultimately, the conversation surrounding Medicaid must transition from one centered on cuts and constraints to one framed around improvement and inclusivity. A serious commitment to addressing the deep-rooted issues facing our social safety nets is crucial. It is time we advocate for solutions that genuinely uplift and support our communities instead of marginalizing those who are already at a disadvantage.